For regular updates, find me on Twitter and Instagram or LinkedIn and find my latest articles on my website.
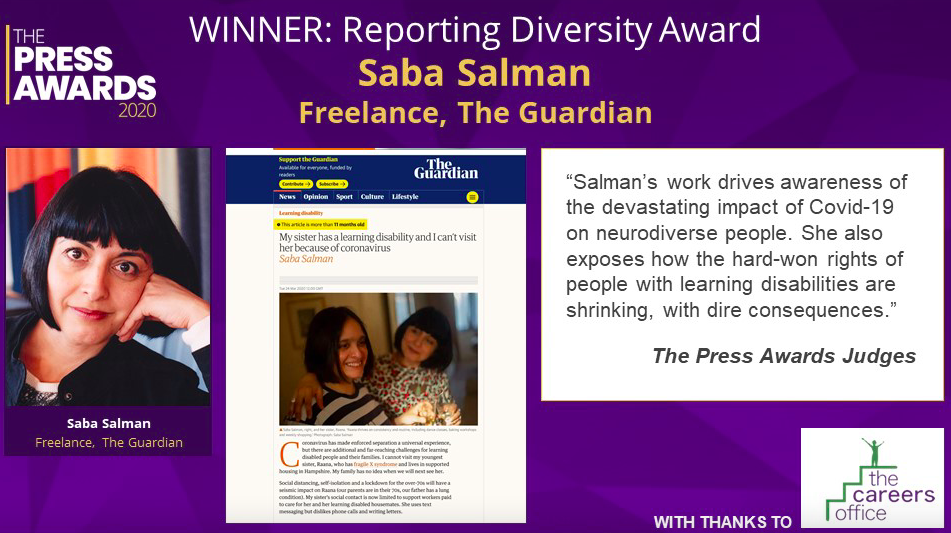
Press Awards 2020 winner
Diversity needs recognition in all its forms, both in terms of who’s doing the reporting and in terms of the issues being reported.
My stories for The Guardian in the Press Awards were commissioned by my former editor Alison Benjamin, and they exist only thanks to people, families and allies who gave time to share words on issues that are too often overlooked.
Much respect to all the journalists I was originally shortlisted with too – I’m in some very fine company.
You can read some of the articles for The Guardian here.
Race and the media

I’ve been thinking since the Harry and Meghan interview and the subsequent debate sparked by the nonsensical claim from the Society of Editors that UK media isn’t bigoted.
An (older, male) editor once asked why I wanted to be an ‘Asian journalist’ when I started out in newspapers (to be clear – the question didn’t need the word ‘Asian’ in it). Later, I was asked to write about arranged marriages as the editor thought this was a topic I ‘must surely know about’. It wasn’t, nor was in my reporting brief, so I declined.
How can any professional body say there’s no bigotry in the sector it represents? There have been so many examples of questionable headlines and reporting, and obviously journalists of colour have had – and continue to have – far worse experiences than the two personal ones I’ve just shared (today, these might be called ‘unconscious bias’?).
The Society of Editors’ board has issued a new statement to clarify the original from Monday. The original ‘did not reflect what we all know: that there is a lot of work to be done in the media to improve diversity and inclusion’.
And that should be diversity of all kinds.
The press awards, in which I was shortlisted for my work on disability issues, have rightly been postponed. Several excellent journalists and news organisations had pulled out, as well as the awards host.
Along with many other journalists of colour, I added my name to two open letters calling for more action on the issue.
Reporting diversity

I’m delighted to have been shortlisted for the Society of Editors’ Press Awards in the ‘reporting diversity’ category.
I’m in fine, strong company in the category and delighted that the Society of Editors is considering the issue of diversity in all its forms.
The articles I’ve been shortlisted for have all been published by The Guardian, and they focus on the brutal impact of Covid on disabled people and their families. The pieces show how the pandemic intensifying the huge inequality already faced by part of our population.
The shortlisted pieces are:
My sister has a learning disability and I can’t visit her because of Coronavirus
Coronavirus restrictions have robbed disabled people of their independence
‘My fear is he’ll never come home’: the learning disabled people locked away in lockdown
I’m privileged to work with people and families and report on these vital issues. I’m also grateful for a supportive, thoughtful and sensitive commissioning editor, Alison Benjamin, who commissioned me to write these articles for The Guardian’s Society pages.
Read more about the awards here.
All learning disabled people should get the covid vaccine

Imagine the anxiety of knowing you are at a greater risk of dying from the Coronavirus but are at the back of the queue for a life-saving vaccination and, if hospitalised, doctors might decide not to save your life.
This is what learning disabled people are facing in this pandemic. They are the hardest hit, yet the impact on their mental health is being overlooked.
I wrote this article for Byline Times on how the government is ignoring the impact of Covid on learning disabled people like my sister Raana.
Covid recovery ignores disabled people

Debates about Covid-19 recovery and economic renewal ignore disabled people. This is shameful given that even before the virus, the UK’s 7.7 million working-age disabled people already faced significant inequalities.
I wrote this opinion piece for the RSA Journal.
The Forgotten Learning Disabled Soldiers of World War One

Arthur Pew was a lance corporal in World War One, serving in the 19th Kings Royal Rifles Corps. Trusted with responsibility for his fellow men, he commanded and organised other soldiers and was a skilled member of a specialist firearms regiment.
Yet, as remarkable new research published today shows, Pew also had a learning disability. And, before he signed up, he was regarded as incapable of contributing to society and was segregated from his fellow men in an institution.
The ‘Hidden History of the Labour Corps in the First World War: Contributions to the War Effort Made by People with Learning Disabilities’ shows how Pew joined the army from an asylum where – in language of the time recorded in the National Archives in Kew – he “was considered to be a mental deficient”.
You can read the full piece in the Byline Times here.
The learning disabled people locked away in lockdown

After a year in secure care 105 miles from home, Jack Cavanagh, 17, who has autism, a learning disability and epilepsy, desperately misses his family. They used to see him every weekend, but with Covid restrictions have been unable to visit. As a result, they say, Jack has become more anxious and isolated and recently begged staff to “be” his mum or dad.
I spoke to several families including Jack’s, about how the use of restraint and isolation has increased during Covid. This group of people have been overlooked during the pandemic despite the fact they are more at risk thanks to the virus.
You can read my Guardian piece here.
Coronavirus restrictions have robbed disabled people of their independence

I wrote a personal piece for the Guardian about how Covid-19 is impacting disabled people and families.
Coronavirus has thrust us all into a new normal. Life has come to feel the same yet different. However, for some communities Covid has undermined their very ethos.
My youngest sister Raana, who has a learning disability, has lived in a supported living community in Hampshire for 10 years. We chose the charity that runs her home for its values. It creates a sense of belonging and purpose, focuses on abilities and is governed by the belief that everyone has the right to be involved in society.
Covid-19 means that not only are the guiding principles of the charity are at risk, but my sister’s independence is being undermined.
You can read the piece on the Guardian website here.
THE SOCIAL ISSUE IS ON A SUMMER BREAK
Back soon…
