I was entranced by some of Cathy Greenblat’s photographs of people with Alzheimer’s, which I came across when researching a recent piece about dementia.
Dementia is a major global challenge – health experts describe it as the next global pandemic. One in three of us will develop it – 135 million people by 2050, according to Alzheimer’s Disease International (ADI), and its annual worldwide health and social-care cost is around £400bn.
Yet Greenblat’s work goes behind the headlines to present the human aspect of the disease.
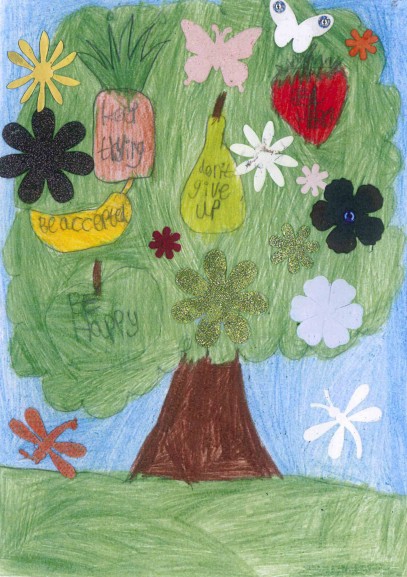
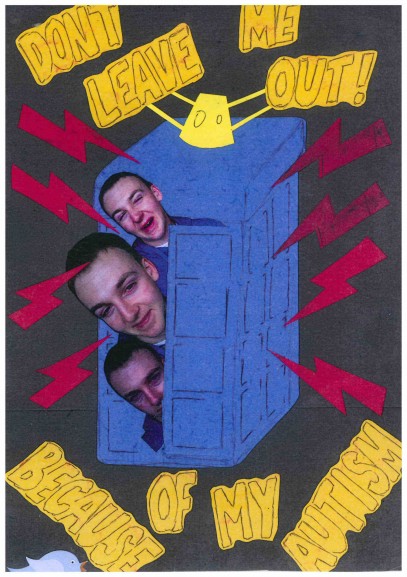
The images in the book Love, Loss and Laughter present a rare view of the illness, shattering the stereotypical image of people as personality-free empty shells, discarded and forgotten by society.

Greenblat’s thought-provoking project to document the lives of people with Alzheimer’s is endorsed by ADI and has taken her all over the world for over a decade (it was published in 2011).
An academic and photographer whose grandparents and mother all developed Alzheimer’s, the sociologist’s work combines a large scale vision and research expertise with a very personal focus on human relationships and societal attitudes. Many of her photographs reveal the characters behind the disease, presenting people with Alzheimer’s in a social or familial context and among friends and carers.
The hundred or so photographs taken in care homes, private houses, clinics and day centres all over the world show how it is possible for people with dementia and their families and carers to experience some joy as they lose their cognitive functions (the “love” and “laughter” in the “loss”). The images show how people can maintain both independence and quality of life.
It is worth pointing out, however, the images do not shirk from touching on the frustration, anxiety and isolation – particularly at the end of life – which Alzheimer’s brings.
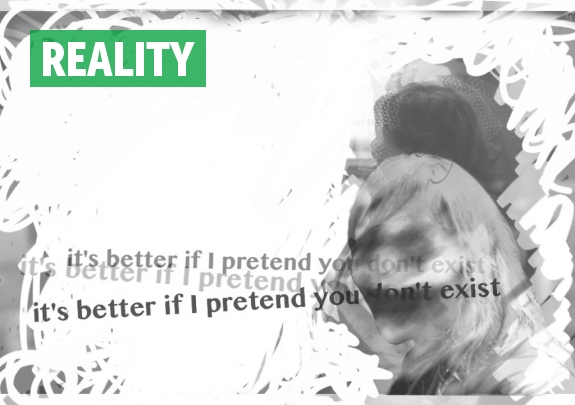
As Greenblat, Professor Emerita of Sociology at Rutgers University, writes in the book, “people with dementia retain vital capacities”. She reinforces the notion that our attitudes to dementia must change if the experience of those with the illness is to improve; her book quotes Michael Verde, president of American dementia organisation Memory Bridge, who says People with dementia don’t disappear unless we disappear from them”. It is possible, as Verde has said, “to change what is referred to as ‘the long goodbye’ into ‘a long hello’”.
The photographer tells me that people are often surprised to hear that the subjects of her pictures have the disease, she says: “I’m often struck by the responses of viewers of my photos at exhibits who ask with some astonishment, ‘But does this person really have Alzheimer’s?” They have only seen images that show people who are sad, dispirited, disconnected, and it takes them time to accept that that is not the necessary condition.
“People who are treated as hopeless lose hope; people who are treated as being unable to do things lose confidence. We don’t treat a sense of hopelessness or lack of confidence with medication: we do it by helping them to feel needed, cared about, being stimulated, communicating differently with them.”
Greenblat will be in Australia in late February to photograph more care settings and explore how to create “joy filled residential communities for people with dementia”. She hope this will result in a multimedia project with interviews, photographs and videos. Some more of her work is included in the gallery below:
• I asked Cathy a few more questions about her work, here’s what she said:
“Perceptions of Alzheimer’s are changing in the time since I’ve been photographing.One of the big changes is that there is so much more talk about Alzheimer’s, in the press, in books of all sorts, on the internet in the form of webinars and connections that are global.
Of importance is the greater participation in the dialogue by people living with dementia – people with diagnoses and people who are their care partners. This is no longer just the medical community telling us about what they know, but sharing of experience…Not everyone is listening to these new voices, but those who do have learned that there are ways to continue a quality life for much longer than has generally been believed.
How has my academic background helped me in my work? Probably the most important thing is that I came to this work with a knowledge of doing research… I knew how to go into new situations and places and learn from people about their lives. Now I was adding a camera to my “tool kit”, as I believe that seeing is so important in changing one’s mind… I speak in an early chapter in the book about ‘Changing people’s minds about people’s changing brains’ – that’s what I have been doing. And I think that is crucial.
I thoroughly believe that we need to distinguish between the physiological changes as we become ill, and the primary symptoms brought about by that. But there are many secondary symptoms such as apathy, aggression, social isolation, that are not caused by the disease but by the way people are treated and come to see themselves .
People who are treated as hopeless lose hope; people who are treated as being unable to do things lose confidence. We don’t treat a sense of hopelessness or lack of confidence with medication: we do it by helping them to feel needed, cared about, being stimulated, communicating differently with them… It is what the photos illustrate. This is not a new perspective… it has been discussed by scholars around the world, but the addition of visual evidence in photos that clearly are not posed has given them wider acceptance.
Many people “run away” from dementia. Surely some people run away from family members or friends who begin acting strangely and are difficult to deal with because they are don’t want to deal with the problem. We all know of siblings who fight about the care to be given to a parent, leaving the responsibility on someone else’s shoulders. They say they are too busy, they had poorer relations before, they have other responsibilities..
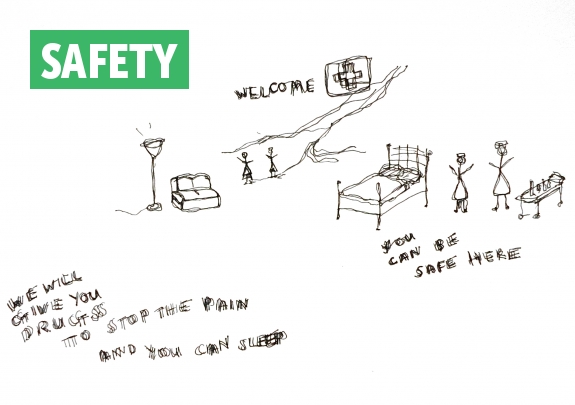
But many people are not selfish and ill informed – rather, they are frightened, they don’t know what to do they don’t know what they can do, they believe that there is nothing that can be done until a cure is found. That is simply not true. There is so much we know how to do now to engage people in continuing stimulating activities. There is so much to be gained through creating partnerships with professionals and other groups that provide day care activities, memory centers, art and music therapy, etc.
We need to help people know that there is a great deal to do and inspire them to find resources near their homes or on the internet. Many friends and family want to be engaged and helpful but they don’t know how to do that. There are excellent books, pamphlets from the Alzheimer’s associations and other groups. This can not only help the person who is ill, but it makes the friends and family feel more empowered… They can learn what to say and how to act in ways that let the person feel they are understood, which in turn reduces the aggression which so often is the result of feeling they can’t clearly express their needs and desires.”
• You can watch some films on Love, Loss and Laughter here and here or visit the website to find out more about upcoming events related to the book and photography project. You can also follow Cathy on Twitter @CathyGreenblat