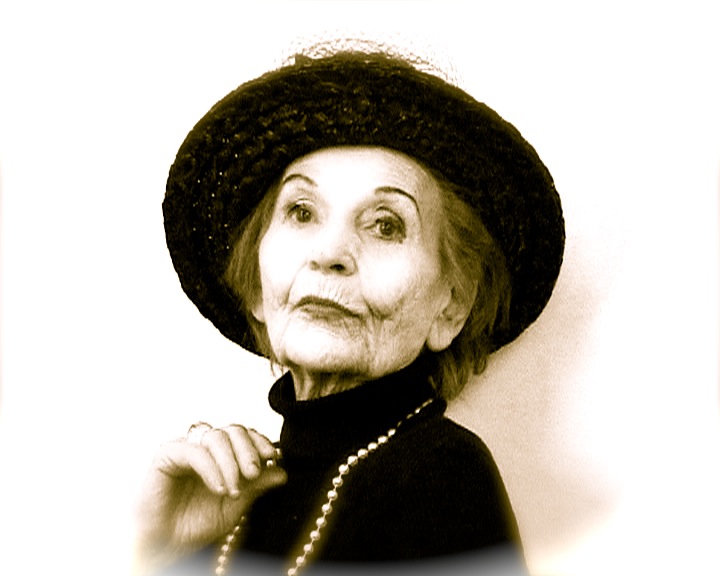
How old does a woman have to be to be categorized as “older”? 50? 70? And if we push females deemed to be “older women”, in “late adulthood” or in “advanced years” into the same group, what common concerns do they share, if any? More importantly, does anyone outside of that demographic notice or care about ageing women? And if they do – what’s being done about the issues they’re concerned about?
While Britain as an ageing society is a constant source of political and public debate, the specific issue of women and ageing isn’t afforded the focus it should, given that women tend to live longer than men. The 2011 census suggests there are about 11 million women over the age of 50 years, about 4 million of which are over 70 years. By 2035 there will be 4 million more females aged 65+ than under 16s.
Like most people, my personal experience – and I speak from the start of my fourth decade – is that the older you get, the younger so-called “older people” seem. As you age, your perceptions of old and young clearly shift. I don’t, for example, class my friends in their 50s as “old” and my own 81-year-old mother-in-law defies stereotypes and expected patterns of behaviour with her far flung travels to South America and her energetic role as a breeder of rare sheep.
The youth/age picture becomes confused still when you think that childhood apparently ends at 12, younger girls are presented (and sometimes present themselves) as much older while older women – think Madonna, Helen Mirren – are variously praised or mocked. And more often than not, the kind of articles I’m thinking of include a particular kind of faux-praise for a woman’s age-defying antics and appearances…you know what I mean – the pieces that comment on a woman’s “confidence” (ie delusion) in “flaunting” (as in “she’s too old to dress/act like that”) her “mature” (read: “wrinkly, untoned”) figure.
A provocative series of essays published today, coinciding with International Women’s Day, highlights policy issues about ageing women, underlining how the contribution to and role of older women in society is overlooked.
The think tank the International Centre for Longevity (ILC-UK) publication Has the sisterhood forgotten older women? contains 38 essays – everything from personal recollections about the role of women in family and society, to thoughts on intimacy and relationships, the invisibility of older women in international development and opinions about the low media profile of older women (see the words of an older female MP on how she is treated by political parties in relation to media work).
The authors include politicians, policy makers, academics and campaigners such as Jane Ashcroft, chief executive of housing and care group Anchor, Sheila Gilmore MP, Michelle Mitchell, chief executive of Age UK, Heléna Herklots from Carers UK and Marina Yannakoudakis MEP.
As well as discussions about how far women in their 50s 60s 70s think of themselves as “old” (answer: they don’t), the collection of writing stresses the dilemma facing older women – while longevity is to be celebrated “there is a risk that women, who often live longer than men, do so at the risk of being caught in the metaphorical mouse trap: alive but with little quality of life”.
The ILC-UK has also today announced it is establishing an Older Women’s Policy and Research Action Alliance to create “a roadmap for future research and policy priorities”. The organisation hopes today’s compedium will spark a new debate on women in an ageing society.
The issue of the challenge for ageing women in care is a particularly strong theme in today’s collection of essays. In the UK, women account for two thirds of community care users over the age of 65, and three quarters of people in residential care.
Baroness Sally Greengross, chief executive of the ILC-UK added: “Women must engage in the debate on social care funding if we are to get a solution which works for all. It is also essential that the caring contributions of older women are not ignored. Future care reform must take account of and not disincentivise the informal care contribution of older women.”
Here are just three edited highlights from among the pieces in today’s publication:
Oh, I didn’t see you there!
Jane Ashcroft, chief executive, Anchor:
“For several years I have been irritated by the propensity of print journalists to tell us the age of any woman in the news, regardless of any relevance to the story, while rarely applying the same approach to men. Why is age a defining characteristic of women?
In 2010, research conducted on behalf of Anchor, the housing and care provider which I lead, analysed one week of TV programmes on the 5 major UK channels (Older Faces Audit, March 2010, Anchor). We found a dramatic under-representation of older people, and especially older women. Across all channels, people over 50 were under–represented. Despite making up 34% of the UK population, representation on the major channels was as low as 12%, with only BBC2 achieving a realistic level of 38%. And amongst TV presenters appearing in the week under review, only 1 in 5 was an older woman.
This supports my view that ageing in men is often seen more positively than in women – many older men are described as wise and experienced, whereas the expression “don’t be such an old woman” is used to convey entirely negative characteristics.
This picture is so different from the reality that I see in my everyday life, that it is tempting to wonder if I live in a parallel universe! Of my 9,000 or so colleagues in Anchor, over 500 are continuing to enjoy their work well past the official “retirement age”.
Behind the scenes, many older women are leading change in communities, organisations and families, contributing their resources and multitude of skills, and leading interesting and rewarding lives. Some older women, like older men, are facing loneliness, loss and poor health. As a society, and for ourselves, don’t we need to recognise every older woman as an individual, and to enable us to do that we need to improve visibility – instead of “oh, I didn’t see you there” can we say “ah, I’ve been looking for you”?
Older women and care: are they invisible to the sisterhood?
Michelle Mitchell, Age UK:
“Despite care having been on the feminist agenda for years, the issue of it in later life has remained shrouded from our viewpoint, as millions struggle in quiet crisis. Yet nowhere are the compound challenges of class, gender and age more evident and nowhere are older women more in need of a voice.”
Older women carers – invisible and ignored?
Heléna Herklots, chief executive, Carers UK:
“Many older women carers grew up during a time when women’s contribution to society was far less recognised than it is today. They now live in a society which too often ignores their contribution as older women carers. We need to challenge this; guard against any prejudices and assumptions we may ourselves have; and work to ensure that older women carers are recognised, respected, and valued – no longer invisible and ignored.”
*Download ILC-UK’s Has the sisterhood forgotten older women? here