Self-harm has always been a taboo subject and in my many years of mental health nursing probably provided more challenges than anything else for me.
It touches at the very core of who we are and how we deal with stress. Our mental strength, or resilience to cope when under pressure, will prevail in many cases but not all.
Recently, new research by the charity YoungMinds suggested that many doctors do not know how to support young people who self-harm. And today comes the news that mental health patients are to be given the right to chose their consultant. As reported today, this will help end what can be a “like it or lump it” service – unlike patients with physical health issues, mental health patients can’t currently chose which psychiatrist they see.
Back to primary care; self-harm is still very much misunderstood by many, and the wider general public. As a mental health nurse, I confess at times to having felt at a loss myself as to how to respond to repeated self harm behaviours. You question your own approach if the problem remains despite intense nursing intervention.
But given that 10 per cent of 15 to 16 year olds are thought to have self-harmed, usually by cutting themselves, if GPs are offering a lacklustre response to the issue (not referring for counselling or for more specific mental health support), this is woefully inadequate.
The mental health charity Mind, suggests that if your GP doesn’t help, you contact the Patient Advice and Liaison Services – and you have a right to change your GP. Mind has some useful practical information on where to get help.
I have worked with some excellent professionals. However, I have also seen others who are in a privileged position to help but who try to look the other way. Or dismiss this as attention seeking behaviour.
In a profession known for its primary focus on the treatment of physical diseases, being presented with a self-harming patient provides an emotional litmus test for many GPs. Why do they get this so wrong sometimes?
Although I don’t want to generalize, I believe that some view this behaviour with frustration and a sense of hopelessness. By this I mean some medical professionals might not feel confident of their own training or understanding to be in a position to deal with things effectively.
Some GPs are too dismissive or refer to mental health services in the knowledge that more specialised knowledge will be available to plan appropriate treatment. Or they automatically reach for the prescription pad to prescribe medication without really asking themselves if a psychological approach would be the more helpful first option.
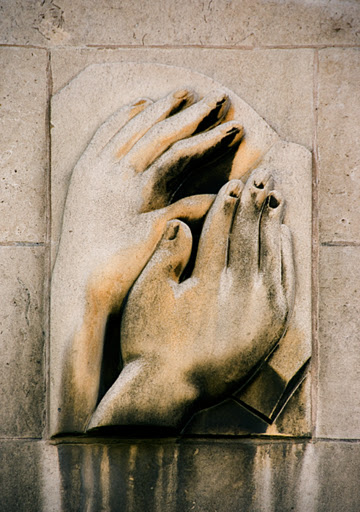
And yet all too often, just a listening ear will help, to allow the person to “offload” within the surgery. This is where the therapeutic relationship between the GP and patient is pivotal to treatment and recovery.
The power of talking openly about concerns face to face cannot be underestimated. A prescription for anti-depressants may be helpful in the long term but we should not rule out even a basic “talking and listening” opportunity as a first option (given GP’s have to stick to set consultation slots, I can see why this might seem an impossible idea – but an approach that encourages people to talk is the right one).
If a person with low self esteem tells the GP they are a “bad person” or “unloved”, the GP can use a simple cognitive behavioural approach of questioning the evidence to support this there and then, of which there is usually very little. And stress to the person that a thought is just a thought, not a fact. Simple but effective initial intervention to encourage someone to question their own negative thought processes.
So what to do?
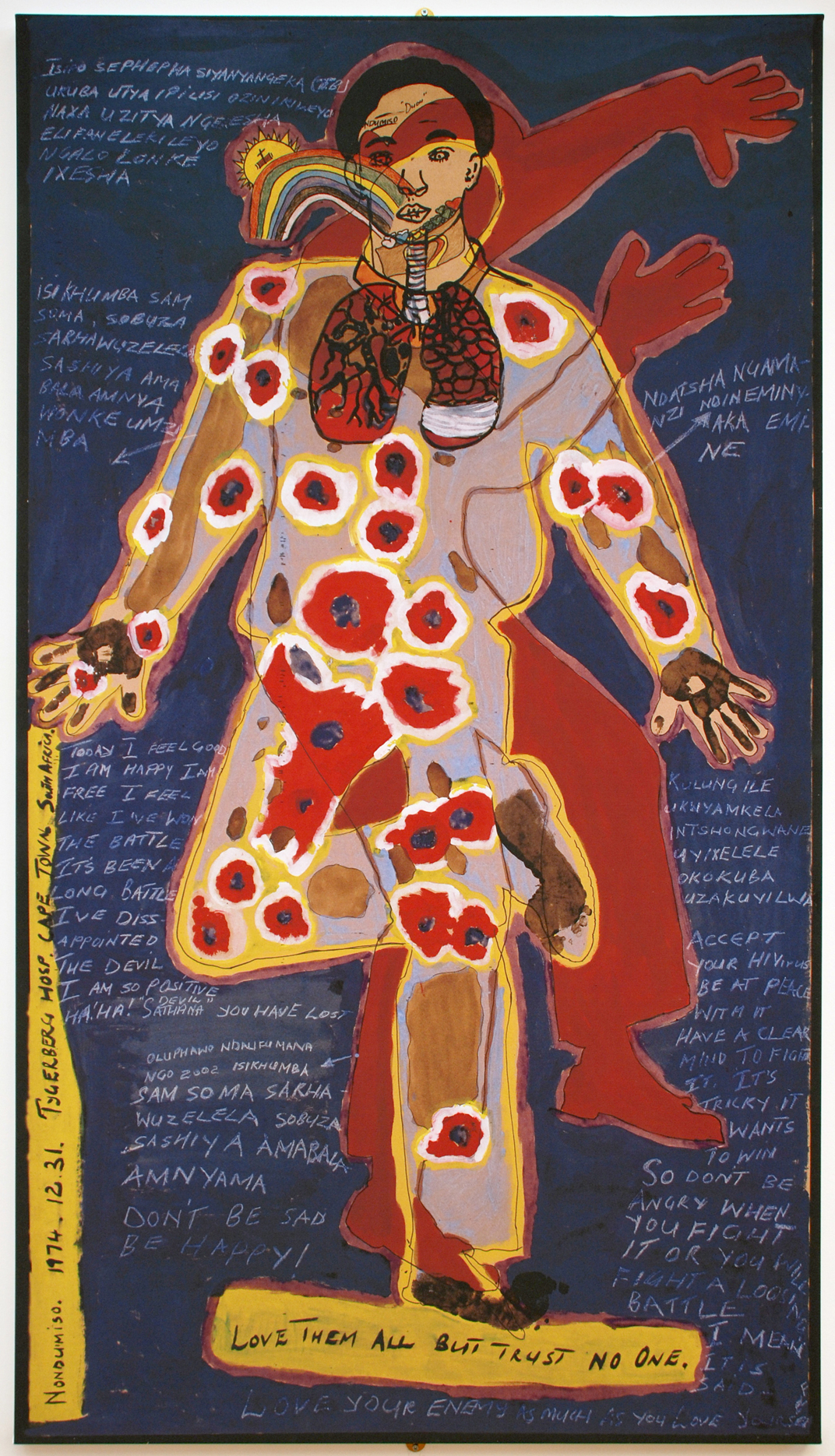
Going back to my opening thoughts, while professionally I’ve found self-harming behavior extremely challenging, one thing I’ve never doubted is my empathy to try to look beyond the physical act of self harm to try to identify its underlining cause.
A behaviour as challenging as self-harm can distract you from seeing the person behind the behavior; what is the emotional conflict driving this kind of behaviour. People can change self-harming behaviours. Being positive and maintaining hope is the starting point of any intervention – and that goes for the professional as well as the individual.