This is where grand ambition contrasts with grim actuality, as I explain in a piece in today’s Guardian.
A report leaked to the BBC and sparked by the preventable death of 18-year-old Connor Sparrowhawk in a Southern Health Trust inpatient unit, revealed that the trust failed to investigate some 1,000 deaths in its care over a four year period.
Then yesterday, the Learning Disability Census Report 2015 from the Health and Social Care Information Centre revealed there 3,000 people in inpatient units – 3,500 if you count those “unreported” in the figures (more on this here from Mencap and the Challenging Behaviour Foundation, and the HSCIC explains the discrepancy under its editors’ note number eight here).
Déjà vu? In 2013, according to the HSCIC, there were also around 3,000 people in inpatient units (in fact half those in units today, were also there for the 2013 headcount). And a previous £2.86m government-funded improvement programme from the Local Government Association and NHS England tried but failed to move everyone out of such units by 1 June 2014.
The census, established in response to the abuse at Winterbourne View, also shows the average length of patients’ stay is five years, there is heavy use of antipsychotic medication (almost three-quarters of people – despite the fact that less than a third have a diagnosed psychotic disorder) and more than half self-harm, have accidents or suffer assault, restraint or seclusion. Around a fifth of all inpatients are at least 100km from home.
Reading these stark facts would lead most of us to conclude that if you have a learning disability, you’re less likely to be cared for properly in life, unlikely to have your premature death investigated thoroughly – but if you’re lucky, you might be included in a census (depending on the data collection methodology etc etc).
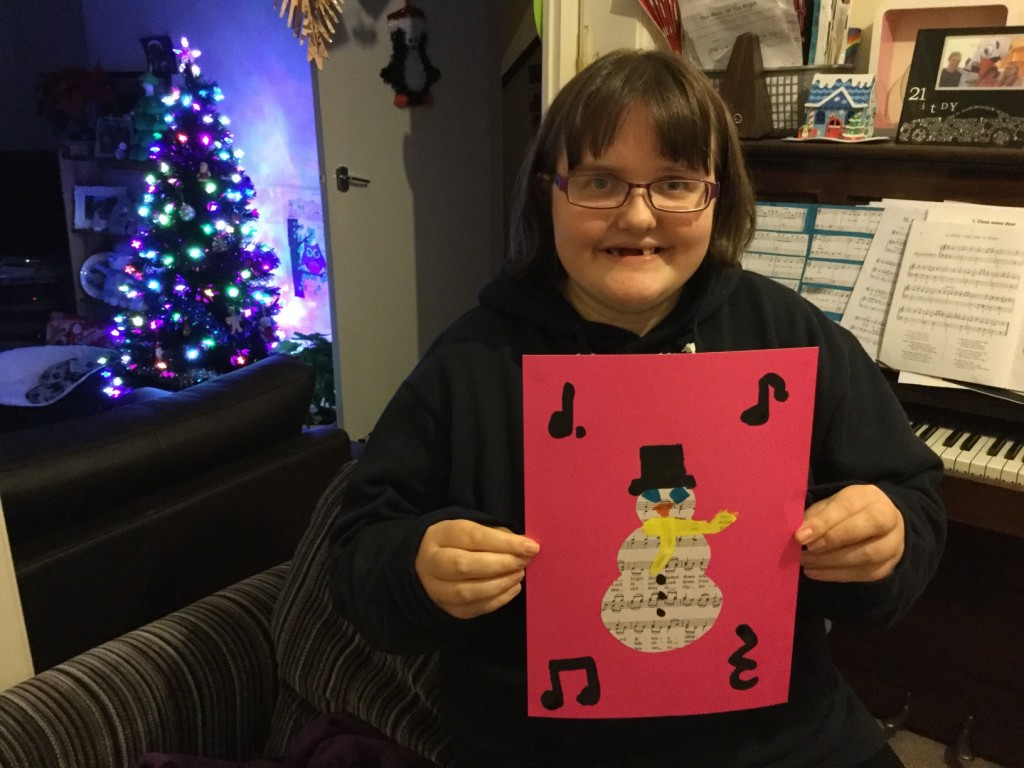
I’m more pragmatic than negative. My sister, Raana, who has a learning disability, leads a busy, active life where her choice is central to her daily life. There are many organisations out there doing great stuff. I’ve met people who have moved from institutions into supported housing in towns and cities, with the help of truly brilliant, hardworking care staff. I’ve spoken to families who feel involved in shaping the care of their son, daughter or sibling, some with very complex needs. I’ve read – and written – reports outlining good practice in ensuring people get out of these places. While there’s still a postcode lottery at play, “we know what good looks like”, as stressed by many social care experts I speak to.
So as I began writing today’s Guardian piece, I’d expected a narrative of cautious optimism. As I came to finishing it, the Mazars report was leaked and new figures showed little change in the number of people in inpatient units, hence the headline above this post.
The report into Southern Health by auditors Mazars – which as I write, is still not published, despite making headlines and being debated in parliament – has renewed concerns over institutional disablism, led to calls for a national inquiry and, as this piece by Andy McNicoll underlines, provoked widespread criticism over the response of the trust and its chief executive (for links to some powerful blogging and commentary, search Twitter for #mazars or #JusticeforLB).
Katherine Runswick-Cole, senior research fellow at Manchester Metroplitan University’s research institute for health and social change, suggests that until the dehumanisation of people with learning disabilities ends, inadequate care – irrespective of care setting – may linger (related issues include, for example, a hospital listing a patient’s learning disability among reasons for sticking a “do not resuscitate” order on his file).
Recent cases in supported living and residential care – non-institutional environments – reflect this concern.
In January, Thomas Rawnsley’s family will attend a pre-inquest meeting into his death. The 20-year-old, who had Down’s syndrome and autism, was taken to hospital from a residential care home in Sheffield earlier this year, but died two days later.
His mother, Paula, says: “Thomas had great empathy and compassion, he always wanted to make people laugh. If people had taken time to get to know him they would’ve found that out.”
Robin Kitt Callender, a care home resident who was severely autistic and partially sighted, with communication difficulties, died on 23 May 2012, less than 24 hours after finally being admitted to hospital. An inquest in March ruled that she died from natural causes contributed to by neglect, with failings by her GP and hospital staff. Robin’s sister Karen has since launched the Casualties of Care campaign for better rights for people and families.
Dismissive attitudes towards people with learning disabilities extend to their families. As Deborah Coles, director of Inquest, has said, the Mazars report only came about “because of the tireless fight for the truth by the family of Connor Sparrowhawk”.
Meanwhile, back with the grand vision – well meaning and welcome as it is – NHS England says it is working closely with regulator the Care Quality Commission to prevent any new assessment and treatment institutions from being created. But in yet more ambition vs. actuality, the Public Accounts Committee has just criticised the CQC for being ineffective.
Connor Sparrowhawk’s mother Sara Ryan, a senior researcher and autism specialist at Oxford University’s Nuffield department of primary care health sciences, says that the Mazars report “confirms that learning disabled people don’t count in life or death” (see more on this on Sara’s blog). And this post by Chris Hatton suggests some “required reading for anyone wanting to understand the issues involved in premature deaths of people with learning disabilities”.
Hard to disagree with the conclusion of Katherine Runswick-Cole who said when I interviewed her, “the pattern is abuse, inquiry, report, repeat”.
